
Todd Paul administers the Johnson & Johnson Covid-19 Janssen Vaccine to Gerald McDavitt, 81, a Veteran of the United States Army Corps of Engineers, at McDavitt’s home in Boston, Mass. last month.
AFP via Getty Images
The United States campaign to reach herd immunity through vaccination involves a delicate — sometimes tricky — dance with side effects, public opinion and virus variants. All three are unpredictable, and can turn when you least expect it.
The rollout of coronavirus vaccines has not been without challenges, but the Biden administration’s strategy of not relying on just one vaccine has preempted potential setbacks with any one product. As recent events illustrate, however, the suspension of one vaccine can impact public opinion of the entire process.
The Food and Drug Administration and Centers for Disease Control and Prevention recommended a pause in the use of the Johnson & Johnson vaccine on Tuesday as they examine six severe cases of rare blood clots. J&J’s JNJ, -1.34% vaccine is an adenovirus vector-based vaccine that only requires one shot. Clinical trials showed it had 72% efficacy in the U.S.
“ ‘It’s still a race between the variants and the vaccine.’ ”
The two-shot mRNA-based vaccines made by Pfizer PFE, +0.51% and German partner BioNTech SE BNTX, +6.68% and Moderna MRNA, +7.40% make up the majority of shots administered in the U.S., and were about 95% effective in clinical trials. (Mayo Clinic research puts their “real world” effectiveness at closer to 88.7%, still high.)
Currently, 22.7% of the U.S. population was fully vaccinated. On Wednesday, the CDC’s Advisory Committee on Immunization Practices will meet to discuss the cases and the FDA has launched an investigation into the cause of the clots.
“It’s still a race between the variants and the vaccine,” Amesh Adalja, a senior scholar at the John Hopkins Center for Health Security and a spokesman for the Infectious Diseases Society of America, told MarketWatch.
Operation Warp Speed, the Trump administration’s vaccine development and distribution program, has been key to this success, he said.
“Part of Operation Warp Speed was not knowing which ones would cross the finish line, and having alternative vaccines that can handle the J&J pause and other vaccines in the pipeline,” Adalja said. “We are increasingly not supply-constrained in the U.S. because of the bulk manufacture of vaccines.”
The FDA and CDC said the J&J pause would give their scientists time to investigate the six cases of blood clotting in vaccinated individuals. There were six cases of cerebral venous sinus thrombosis, a blood-clotting disorder, out of roughly 6.8 million people in the U.S. who have received this vaccine.
“When I was offered Moderna, J&J wasn’t even an option. It was never in my consideration not to take it,” Maury Newburger, a New York-based travel consultant who received the Moderna vaccine in March. “Knowing what I know now, I probably would not take the J&J. I still think I would have taken the two-shot vaccines.”
All six cases of blood clots occurred in women ages 18 to 48. One woman died, and another remains in critical condition, according to details released by the FDA Tuesday. “We are recommending a pause in the use of this vaccine out of an abundance of caution,” health officials said.
“Hiccups in production and hiccups in safety are inevitable,” said Dr. Andrew Pavia, the George and Esther Gross Presidential Professor at the University of Utah and chief of the Division of Pediatric Infectious Diseases.
“It was a wise decision to spread the risk,” he told MarketWatch. “Factories can be hit by a hurricane, run out of a supply, or be hit by contamination that forces them to shut down.”

Maury Newburger in Greenland in before the coronavirus pandemic. He received the Moderna vaccine in March. ’Knowing what I know now, I probably would not take the J&J,’ he said.
c/o Maury Newburger
The good (and the bad) news
The good news: Pfizer-BioNTech and Moderna supply the majority of vaccines in the U.S., and currently ship roughly 23 million doses a week here. The White House said the J&J pause will not have a “significant impact” on the rollout in the U.S.
”We’ve been doing fairly well and not having the outcome Europe is having,” Adalja said. “We have successfully vaccinated high-risk populations: nursing-home residents and those in community dwellings. We’re nowhere near the winter surge. Nursing-home deaths have plummeted.”
White House COVID-19 response coordinator Jeff Zients said in a statement: “This announcement will not have a significant impact on our vaccination plan: Johnson & Johnson vaccine makes up less than 5% of the recorded shots in arms in the United States to date.”
“ ‘These types of things make vaccine-hesitant people more concerned.’ ”
The latest complication has further delayed a rocky rollout in the European Union, which ordered approximately 200 million doses of the J&J vaccine in 2021. “We have made the decision to proactively delay the rollout of our vaccine in Europe,” J&J said in a statement Tuesday. The U.K. has ordered 30 million doses of the J&J vaccine, although it has not yet been authorized for use there.
Now, for the bad news: “Unfortunately, there is always going to be a halo effect in a negative way,” Dr. Aaron Glatt, the chair of the department of medicine at Mount Sinai South Nassau in Oceanside, N.Y., told MarketWatch. “What’s happened with J&J is forcing people to have questions with all vaccines.”
The J&J vaccine “remains an extremely important vaccine for a fatal disease,” he added. “These types of things make vaccine-hesitant people more concerned.”
“Certainly, having other vaccines has been extremely helpful because there can always be manufacturing issues, or different strains may or may not be effective against a particular vaccine. That’s not intentional, it’s just the way science works,” Glatt said.
“The boosters, if and when they do come, will be more easily approved,” he added. “We’ve done most of the legwork already. It’s impossible to predict what will happen. It’s possible the vaccines will have efficacy against different strains. Time will tell, and the different strains will tell as well.”
In one recent Kaiser Family Foundation poll taken before the J&J vaccination pause, 13% of Americans said they would definitely not get the vaccine, and 7% said they would get it only if required.
“As humans, we are not very good at translating risk into action,” Pavia said. “If I have the chance of being one of the 500,000 who die of COVID, how do I balance that with the one person who had a fatal side effect, if it’s a side effect at all? It’s the same perceptual problem when we blindly drive to the airport texting, yet we worry about the airplane.”
In the aftermath of the J&J vaccine pause, Barbara Alexander, president of the Infectious Diseases Society of America, said that the American public must continue to receive clear, accurate and up-to-date information, and have their questions answered, “so that we can maintain and build trust and confidence in COVID-19 vaccines.”
“The risk of becoming infected with COVID-19, and the potential for severe illness or death, remains a serious concern, and we urge everyone who is eligible to take the opportunity to be vaccinated with one of the currently available options,” she added.
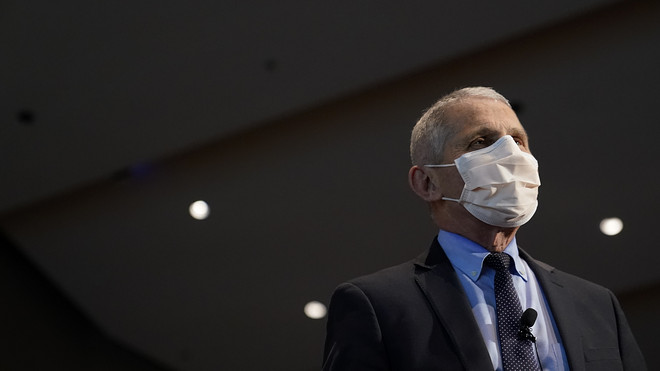
Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases, has said good ‘herd immunity’ would equate to 70% to 85%, and that the U.S. should start to see a return to normalcy by the fall.
Getty Images
The appeal of J&J and AstraZeneca
The J&J blood-clot issue is similar to one that caused many European countries to pause and/or restrict use of the AstraZeneca AZN, -0.47% and Oxford University coronavirus vaccine, which is also an adenovirus viral vector-based vaccine. The U.K. has restricted its use to those over age 30.
Moderna started its vaccine rollout in England on Tuesday, providing an alternative to the AstraZeneca vaccine. In Ireland, where Pfizer-BioNTech and Moderna are also available, authorities decided to limit AstraZeneca to people over age 60 for the same reason.
The AstraZeneca vaccine was appealing for poorer countries and rural communities, said Bill Schaffner, professor of medicine in the Division of Infectious Diseases at the Vanderbilt University School of Medicine, Nashville, Tenn.
“ ‘We’re not going to get COVID zero. It’s going to be with us season after season.’ ”
“AstraZeneca was supposed to be a relatively inexpensive vaccine, and it can be handled at conventional refrigerator temperature,” he said. “That issues with this vaccine is putting a substantial crimp into the plans of distributing it internationally.”
The J&J vaccine, meanwhile, was an attractive prospect for people who had a particular dislike of vaccines and/or needles, Schaffner added.
“The J&J vaccine has kind of caught on because it’s one and done, so this pause will no doubt slow us down,” he said. “In our state, as we try to vaccinate more people in rural areas, we’ve run into real vaccine hesitancy or indifference to getting vaccinated.”
Elsewhere, Russia’s Gam-COVID-Vac (Sputnik V) coronavirus vaccine was the first in the world to be approved last August, and Hungary was the first country in the European Union to approve it. That country too has rolled out more vaccines. A second Russian vaccine, EpiVacCorona, was registered in October. Last month, Russia approved a third domestic COVID-19 vaccine, CoviVac.
The number of deaths from COVID-19 in the U.S. has reached 563,428, and continues to climb. More than 31.3 million people in the U.S. have been infected by the coronavirus since the pandemic began. Worldwide, more than 2.9 million people have died from the disease.
Anthony Fauci, the director of the National Institute of Allergy and Infectious Diseases, has said that good “herd immunity” would equate to 70% to 85%, and that the U.S. should start to see a return to normalcy by the fall. That, of course, depends on individuals’ age, circumstances and underlying conditions.
“Herd immunity is likely something that will happen in late summer,” Adalja said. “We’re not going to get COVID zero — it’s going to be with us season after season, but it’s not going to have the ability to cause a public-health emergency. The key was to tame it, and the damage it was causing.”
Vaccine variety also helps protect against variants. Israel has vaccinated over 50% of its population so far. A preprint of a small study, which was published last Friday, said the B.1.351 coronavirus variant, first detected in South Africa, was more likely to infect people in Israel who had been vaccinated with Pfizer’s vaccine.
The study has not been peer reviewed, but it was still of particular interest in Israel, which has relied predominantly on the Pfizer/BioNTech vaccine.
Fauci said clinical data thus far indicates the mRNA vaccines developed by Pfizer and BioNTech and Moderna provide protection against B.1.1.7, first detected in the U.K., but their efficacy is thought to drop against the B.1.351 variant, a rarer strain of the virus, at least in the U.S.
Newburger, the travel consultant, never got a flu vaccine until the coronavirus came along. “I never did believe in the flu shot,” he said. “I maybe got sick one or two days a year, but this was the first year I got the flu shot. It was the combination of COVID, traveling and the possibility of catching something, and this time I thought, ‘I’ll get it.’”
He said there will always be vaccine holdouts who remain beyond convincing to any coronavirus vaccine. “There’s a very small group of people who don’t believe in it for religious reasons or political reasons, or they’re just completely oblivious,” he said. “That’s hard for me to comprehend.”
